Central Motor
Conduction Time (CMCT) is a neurophysiological parameter that measures the time
taken for a motor impulse to travel along the central motor pathways from the
motor cortex to the spinal motor neurons. Here is a detailed explanation of
Central Motor Conduction Time:
1. Definition: CMCT is a
measure of the conduction time through the central nervous system, specifically
along the corticospinal tract, which is responsible for voluntary motor
control. It reflects the integrity and efficiency of the neural pathways
connecting the motor cortex to the spinal cord and peripheral muscles.
2. Methodology:
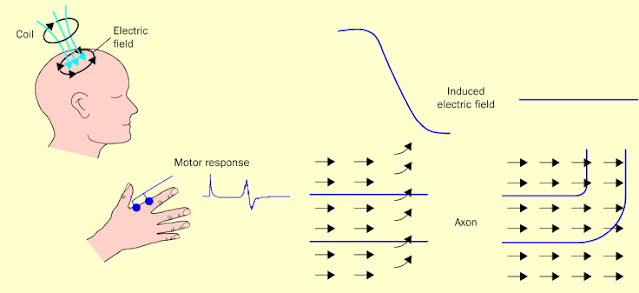
o Stimulation: CMCT is
typically assessed using transcranial magnetic stimulation (TMS) to stimulate
the primary motor cortex and evoke motor responses in the target muscles. The
timing of the motor evoked potentials (MEPs) elicited by TMS is measured to
determine the conduction time from the cortex to the muscles.
o Recording:
Electromyography (EMG) recordings are used to capture the MEPs in the muscles
of interest. By analyzing the onset latency of the MEPs relative to the TMS
pulse, researchers can calculate the CMCT, which includes the time for synaptic
transmission, conduction along the corticospinal tract, and neuromuscular
junction transmission.
3. Significance:
o Motor Pathway
Integrity: CMCT
provides information about the functional integrity of the central motor
pathways, including the corticospinal tract. Prolonged CMCT may indicate
disruptions or abnormalities in the neural conduction along these pathways,
which can be associated with neurological conditions affecting motor function.
o Diagnostic Value: Changes in CMCT
can be observed in various neurological disorders, such as multiple sclerosis,
motor neuron diseases, and stroke. Monitoring CMCT alterations can aid in
diagnosing and monitoring disease progression, as well as assessing the effects
of therapeutic interventions.
4. Clinical
Applications:
o Neurological
Disorders: CMCT
measurements are used in clinical neurophysiology to evaluate motor pathway
function in patients with neurological conditions affecting the central nervous
system. Abnormal CMCT values can indicate underlying pathology and help guide
treatment decisions.
o Research: CMCT
assessments are also valuable in research settings to investigate motor system
physiology, plasticity, and adaptations in response to interventions such as
rehabilitation, pharmacological treatments, or neurostimulation techniques.
Studying CMCT can provide insights into motor control mechanisms and neural
plasticity.
In summary,
Central Motor Conduction Time is a neurophysiological parameter that assesses
the conduction time along the central motor pathways from the motor cortex to
the muscles. By measuring CMCT, clinicians and researchers can evaluate the
integrity of the corticospinal tract, diagnose neurological disorders affecting
motor function, and monitor changes in motor pathway function over time.

Comments
Post a Comment